15 Causes Of Bumps On The Face + Best Treatments, From Derms


Picture this: You’re cleansing your face at night and feel a bump. Your immediate reaction may be to slather it in spot treatment and assume it’s a zit, but is that actually the best route?
Unfortunately, bumps on your face aren’t always what they appear to be. In fact, there’s a long list of potential causes, and thus, a long list of different treatment routes. To find out which bump you’re dealing with, you’ll need some context clues.
Advertisement
To help you out, we asked dermatologists for a full guide to bumps on the face. Below, the must-know traits of each cause and how to treat them.
Closed comedones or whiteheads

First up we have whiteheads. “A white head (also known as closed comedones) is a hair follicle or pore that has become clogged with oil and dead skin cells," board-certified dermatologist Lian Mack, M.D., FAAD, previously told mbg.
Most whiteheads tend to be flat compared to other forms of acne, and as you might expect, have a white top instead of a blackhead. These won’t have tons of redness around them like other pimples, and they shouldn’t be as tender to the touch as a standard zit.
You’ll most often find whiteheads around oily parts of the face like the chin, forehead, and nose. Anyone with oily skin will be more prone to whiteheads, but any skin type can get them from time to time.
Whiteheads are caused by a combination of factors including oil buildup, dead skin buildup, pore-clogging ingredients, hormonal imbalances, diet, and even some hair care products.
Advertisement
How to treat comedones
When it comes to whitehead remedies, "Retinoids fall at the top of the list," Mack said. "Retinoids are vitamin A derivatives that reduce oil production and promote cellular turnover," she explained.
"This treatment works well because whiteheads are caused when sebum and dead skin cells unite to clog a pore," she added. You can find retinol in many over-the-counter forms such as classic retinol, retinaldehyde, and adapalene. Or, chat with your dermatologist about prescription-grade formulas.
Apart from retinoids, look to the following options:
- Salicylic acid
- Benzoyl peroxide
- Clay masks
- Get an acne facial
Advertisement
Products for whiteheads
Inflamed acne
If it’s more inflamed than a whitehead but still looks like a pimple, it’s probably just that: Inflammatory acne. Two common forms of this type of breakout include papules and pustules.
"Papules look like solid red bumps, while pustules have pus at the top," board-certified dermatologist Zenovia Gabriel, M.D., FAAD, previously said.
Papules often turn into pustules. When the red papule forms a white, pus-filled head, you now have a tender pustule. People often mistake this white head as, well, a "whitehead," but in clinical derm-speak, those are two very different things.
Also like other breakouts, this type of acne can be linked to your lifestyle including your diet, exercise habits, stress levels, and hormones. If you think those may be at play, consult your dermatologist.
Advertisement
How to treat inflamed acne
Like any form of acne, there are a few different treatment routes you can take. Below, a quick breakdown of the best ones for this specific type of pimple:
- Benzoyl peroxide
- Tea tree oil
- Chamomile
- AHAs & BHAs
- Use a spot treatment overnight
- Ice your pimple for 30 seconds to relieve redness
Advertisement
Products for inflammatory acne
Cystic acne

Cystic breakouts (also known as blind pimples) is a form of inflammatory acne, but it’s much different from the zits discussed above. If your bump appears red and doesn’t come to a white or black head, you might have a cystic breakout. Cysts are often tender, and may even feel soft to the touch.
Cystic acne tends to be red, inflamed, and larger than other breakouts. The giveaway that you've got a cystic breakout? You can feel it below the skin, but the only evidence on the surface is a red mark and raised bump.
This form of acne is very difficult to treat with just over-the-counter products, especially if it’s consistent. Your first step should be to visit a dermatologist if you can to get ahead of possible scarring that can follow long term cystic breakouts.
The reason it’s so complex is because it’s often linked to factors like genetics, hormones, stress, diet, and gut health—all things OTC skin care products won’t address.
How to treat cystic acne
Below, common treatments for severe cystic acne:
- Retinoids: Cystic acne often calls for prescription-grade retinoids like tretinoin, but you can try an OTC product first. Look for retinaldehyde or adapalene—two stronger form of retinol that are available without prescription.
- Spironolactone: While spironolactone was originally used for heart failure and high blood pressure, it has proven to be an effective treatment for hormonal acne in women, with minimal bothersome side effects.
- Isotretinoin: Also known as Accutane, isotretinoin is an oral medication dermatologists prescribe for patients who have had consistent, treatment-resistant cystic pimples. It’s a serious drug with important side effects to be aware of and requires many doctor visits. If you have consistent cystic acne, ask your doctor about isotretinoin before assuming it’s right for you.
Acne scars

If you feel a bump on your skin that actually just looks like skin, it may be an acne scar. The obvious giveaway would be that you’ve had acne in the past.
There are many different types of acne scars (reference our graphic for this one) including those that are divots in the skin, and bumps or rough spots on top of the skin. If you’re feeling a raised scar, it may be a keloid.
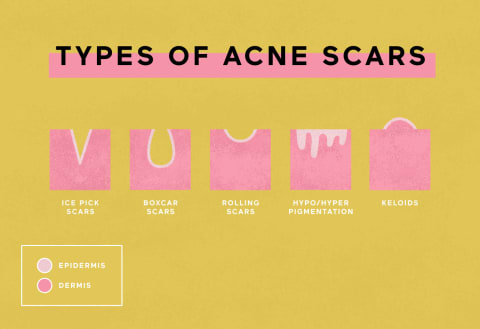
Keloids and hypertrophic scars1 occur because there's an excess of scar tissue. These form as the result of acne as well as just general injuries. These appear more frequently from body acne, but can show up on the face, too.
Keloids and hypertrophic scars take dermatologic intervention, and there's not much you can do on your own. Also: If you develop them once, it likely means you are at risk of at developing them again22, so get it checked out ASAP if you can.
How to treat acne scars
If you have a different kind of acne scar (read: not a keloid), then look to the follow ingredients to ease the appearance:
- Retinol
- Glycolic acid
- Salicylic acid
- Lactic acid
Dive deeper: How To Get Rid Of Acne Scars, From Dermatologists
[products]
Rosacea

If your bump is accompanied by loads of redness, you may be dealing with rosacea. “It commonly causes redness and visible blood vessels on the central face—the nose, medial cheeks, forehead and chin,” says board-certified dermatologist Hadley King, M.D., FAAD.
She adds, “There may also be small red, pus-filled bumps or in severe cases, coarse changes in the skin.” Some people with rosacea experience constant flushing, while others may be even-toned one minute and super red the next.
This sudden flushing is due to rosacea triggers, which are different from person to person. However, there are some common triggers out there, so read through the following list from the American Academy of Dermatology and try to remember (or take note for the future) if your face flushes from these events:
- Drinking alcohol
- Hot temperatures
- Aerobic exercise
- Using saunas & steam rooms
- Eating spicy foods
- Excessive sun exposure
- Using hairspray
How to treat rosacea
Treating rosacea as an overarching skin condition will help to ease rosacea bumps. The first step is to avoid your triggers, but that’s definitely easier said than done. So, couple those efforts with topical care.
It’s important to note that with rosacea, your skin barrier is compromised. Because of this, many of the products and practices you call upon should be focused on soothing, hydrating, and healing that barrier.
Below, some tips for treating rosacea:
- Use azalaic acid: “Azalaic acid is also helpful, as is sodium sulfacetamide for its anti-inflammatory properties,” King says.
- Look for ceramides: This ingredient is both healing, hydrating, and soothing all at once. Look for ceramides in your cleansers, moisturizers, and serums.
- Talk to your derm: There are many more topical treatments available with a prescription, so visit your derm if your at-home remedies aren’t working. In addition, dermatologists can provide IPL laser treatment, which King notes is particularly helpful for easing redness in patients with rosacea.
Products for rosacea
Eczema
If your bump is alongside dry and flaky skin, it may be eczema. “Eczema can appear in many different forms, sometimes just as dry, itchy skin, sometimes as bumps around hair follicles, and sometimes as an itchy, inflamed and bumpy rash,” says board-certified dermatologist and Co-Founder of Fig.1 Courtney Rubin, M.D., FAAD.
“Bumps from eczema typically do not have pus inside the way that acne or rosacea bumps do,” board-certified dermatologist Dustin Portela, D.O, FAAD explains.
You may notice your eczema (and therefore the bumps) flare in times of high stress, or in dry and cold weather conditions.
How to treat eczema
The main goal in treating eczema is to support the skin barrier, ease irritation, and minimize inflammation. To do so, look for rich hydrating creams and do your best to stay away from irritants.
Everyone is different, but many people with eczema are sensitive to fragrance, exfoliants, and retinol—so put those aside if you’re in the middle of a flare up. Instead, look for fragrance-free moisturizers with the following ingredients:
- Coconut oil
- Ceramides
- Oat oil
- Hyaluronic acid
- Glycerin
- Vitamin E
- Shea butter
- Aloe vera
Products for eczema
Psoriasis
Psoriasis is another skin condition that has similar symptoms to eczema. You may see dry and flaky patches alongside raised bumps, but the psoriasis patches and bumps will be more red, whereas eczema is generally skin color and slightly pink or red when irritated.
According to the Centers for Disease Control and Prevention (CDC)3, “Psoriasis is an autoimmune disease, meaning that part of the body’s own immune system becomes overactive and attacks normal tissues in the body.”
Psoriasis often flares during times of high stress and when your immune system is otherwise compromised by a cold, virus, etc.
Unfortunately, this means there isn’t a whole lot you can do about it at home. If you think you have psoriasis, it’s best to visit a dermatologist to be sure and get the best treatment available to you.
How to treat psoriasis
At home care is similar to that of eczema. According to the AAD, these are the best tips to follow:
- Use fragrance-free products
- Choose creams, ointments, and oils over lotions
- Use calamine products to ease itch
KP
Often referred to as KP, keratosis pilaris is most common on the back of the arms, but can be found on the legs and face as well.
“Keratosis Pilaris (KP) bumps are often called ‘chicken skin’ as they are small, red, and resemble chicken skin,” says board-certified dermatologist and Co-Founder of Skintensive Anar Mikailov, MD, FAAD.
KP shows up more on the cheeks and jaw area than the T-zone, Mikailov says. It’s caused by a buildup of keratin, but new studies show that KP may also be caused by a lack of oil-producing glands4, he adds.
Your dermatologist may be able to help you identify KP, but there isn’t a cure for it yet. However, there are steps you can take to manage it and minimize its appearance.
How to treat KP
Because of the dual mechanism cause, it’s important to address both needs via exfoliation and nourishment. Below, a few tips from Mikalov:
- No sugar scrubs: “Avoid any scrubs using sugar, coffee grounds, or walnut beads; find exfoliators made with jojoba wax esters.”
- Nothing over 7% AHA: “For those looking for chemical exfoliators, avoid anything over 7% AHAs.”
- Try PHAs: “If possible, look for products formulated with PHAs instead as they are much more gentle on the skin.”
- Don’t skip moisturizer: “When using coconut oil, squalane, and jojoba oil, the majority of individuals with KP will see improvement.”
Products for KP
Contact dermatitis
Next, you have contact dermatitis. This one is complex, but also common. Mild cases result in patches of slightly bumpy, red, or irritated-looking skin, often with some mild flaking, like an angry skin goatee.
With more severe cases, skin becomes very inflamed, with flakes or scabs that can bleed and become infected.
Your skin may feel sensitized, even to non-irritating skin care products—a sign it could be dermatitis or another type of reaction.
One common form of dermatitis is perioral dermatitis, which shows up around the mouth. So if your bumps are only around your lips and chin, that may be the specific situation you’re dealing with.
How to treat contact dermatitis
You can get dermatitis from many things—from stress to overuse of retinol to food intolerance and beyond. This one can be difficult to completely heal at home, so visit a derm if you think you do have dermatitis.
As far as at-home remedies go,though, just stick with hydrating and soothing products. Below, a few things to avoid that could trigger a flare-up:
- Fragrance in skin care
- Retinol
- Chemical exfoliants
- Spicy food
- High stress
- Inflammatory foods
Milia

Say your bump is tiny, white-ish, and near your eyes. Chances are, you have milia. Unlike acne, milia are not caused by an infection in the pore.
Elena Villanueva, D.C., founder of Modern Holistic Health previously told mbg that milia is actually a buildup of keratin that gets trapped beneath the surface of the skin.
It's also important to know that, unlike acne, milia does not get inflamed, red, or swollen. And you don't have to have acne-prone skin to develop milia. In fact, people with dry or dehydrated skin are even more prone to milia.
How to treat milia
First, you should know that removing milia at home is a huge no-no. If you want the bumps to go away quickly, follow these steps:
- Stop using eye cream for a week: Many people get milia around their eyes when using eye cream religiously, and it may go away if you stop using it. This is an anecdotal connection, but still one worth noting nevertheless.
- Use gentle exfoliants: Use salicylic and glycolic acid to exfoliate the area. When looking for a formula, keep an eye out for low-potency exfoliators to ensure you keep the skin barrier intact when exfoliating.
- Visit a derm: If the bump really bothers you, your dermatologist may be able to extract it.
Ingrown hairs
“Ingrown hairs typically appear as a raised red bump that is often painful to the touch,” Portella explains. They may look like a tiny pimple in some cases. On occasion, you can actually see a hair stuck in the inflamed bump.
“Ingrown hairs can happen anywhere shaving or plucking occurs, usually on the chin and jawline, and appear as inflamed bumps with a hair in the middle that has turned in on itself,” Rubin says, which is why they’re more common in those who shave their face.
Regular exfoliation and exfoliation before shaving can help to prevent ingrown hairs from happening on a regular basis. In addition, be sure to switch out your razor frequently as dull blades are more likely to cause ingrown hairs.
How to treat ingrown hairs
Most ingrown hairs will go away on their own within a few days. In the meantime, try using a warm compress and ingrown hair spot treatment. It’s also important to refrain from shaving in this area until the ingrown hair has healed.
Products for ingrown hairs
Moles

If you’ve had this bump for a while and it’s not sensitive or changing, it could just be a mole. “Moles are often brown, but not in all cases,” Portella says. “In some individuals, they are more likely to have flesh colored or even slightly pink or red moles,” he adds.
You’ll know it’s a mole if it’s not sensitive, it doesn’t come to a head, and it doesn’t seem to be filled with anything. Also, moles can appear quite quickly on the skin if you’ve been spending loads of time in the sun, so don’t be surprised if it seems to pop up out of nowhere.
How to treat moles
Unproblematic moles don’t call for treatment, unless they bother you aesthetically. Still, it’s important to have your moles checked every year at least to ensure you catch any potential skin cancer early.
“If you have a cosmetic concern about the appearance of a mole, see a board certified dermatologist first to evaluate whether the mole appears healthy and normal,” Rubin says.
If you do want to remove the mole, your dermatologist can determine the best method.
Lipomas

If the bump is totally under the skin, but not exactly looking like a cyst, it could be a lipoma.
“Lipomas can appear as soft or firm nodules (balls under skin) and are usually mobile (can feel like they are rolling under the skin, not fixed) bumps or nodules, which can vary in size,” says board-certified dermatologist and Director of Cosmetic Dermatology at Montefiore Advanced Care Kseniya Kobets, M.D., FAAD.
Most of the time lipomas aren’t painful or itchy, unless they’re located on parts of the body that get easily irritated. If left alone, they can grow quite large over time. They may seem serious due to the size and strange feel, but most of the time they’re not a health concern.
How to treat lipomas
“Although lipomas that are not bothersome do not need to be treated, definitive treatment for lipomas is surgical removal that involves local anesthesia shots and leaves the area with a linear scar,” Kobets says.
In short, you should definitely visit your doctor if you suspect you have a lipoma. This doesn’t mean you have to remove it, but it’s a good idea to know what it is regardless.
Hives

“Urticaria, or hives, is an outbreak of swollen, pale red bumps or wheals on the skin that appear suddenly,” King notes. “They usually cause itching but may also burn or sting,” she adds.
Hives naturally go away within 24 hours, and the entire outbreak should resolve within days to weeks, she adds.
“Hives can result from the body's reaction to certain allergens, or they can happen for unknown reasons,” King says. This could be topical allergens in skin care products, something you ate, something in the air, and so on.
High stress situations can also trigger hives, or make present hives worse.
How to treat hives
“Because hives are triggered by a release of histamine, oral antihistamines are generally the most effective treatment,” King says. In the moment, it’s better to just let your hives be than slather any cream on them.
To prevent future hives, try to avoid allergic triggers. If you frequently get hives, consider keeping a note page on when you get them and what you were exposed to beforehand to trace a possible allergy.
Those prone to frequent hives may consider taking an oral antihistamine (AKA allergy medicine) on a daily basis. If you’re not sure, speak with your doctor.
Infection
Last but not least, we have general skin infections. Now your bump could be caused by something else and then get infected, or it can be a sign of an infection to begin with.
“If a bump starts to blister, ooze yellow or green pus, have yellow crusting, or is associated with pain and swelling, it could mean that it’s turning into an infection,” Kobets says.
One common infection is impetigo. “Impetigo is a bacterial skin infection that can have honey colored crust, which can sometimes happen with worsening eczema or infected hair follicles,” Kobets says.
You could also have cold sores which start off as red, painful, burning, or itchy bumps and progress into fluid-filled blisters that crust over, she adds.
Chickenpox is another virus in the herpes family and typically affects children who are not vaccinated for it. It’s rare to have chickenpox only on the face and not the body, so that’s one major giveaway.
How to treat infection
If you think you have an infection of any kind, visit your doctor. Common skin infections like impetigo are highly contagious (to other body parts and other people), so it’s best to get help sooner rather than later.
In the mean time, just don’t touch your infected bump. If you accidentally do touch it, wash your hands afterward with soap and water to prevent spreading the potential infection.
Once you visit your doctor, they may give you antibiotics or topical treatment creams and ointments. This one is quite serious, so don’t take it lightly.
FAQ
How do I get rid of small bumps on my face?
The first step to treating bumps on your face is identifying what the bump is. Common bumps include pimples, milia, ingrown hairs, and hives. Other skin conditions like eczema, rosacea, and psoriasis can also result in bumps. There are plenty of other causes for bumps on the face, so visit your dermatologist for help.
What causes bumps on face that are not pimples?
Common bumps include pimples, milia, ingrown hairs, and hives. Other skin conditions like eczema, rosacea, and psoriasis can also result in bumps. There are plenty of other causes for bumps on the face, so visit your dermatologist for help.
What are the bumps on my face called?
Common bumps include pimples, milia, ingrown hairs, and hives. Other skin conditions like eczema, rosacea, and psoriasis can also result in bumps. There are plenty of other causes for bumps on the face, so visit your dermatologist for help.
The takeaway
As you can tell, a bump on the face could be many things. Before you go in heavy handed with any kind of treatment, consider the additional symptoms you’re experiencing, and take note of what the bump looks like in detail. When in doubt, ask your derm.

Hannah Frye is the Assistant Beauty Editor at mindbodygreen. She has a B.S. in journalism and a minor in women’s, gender, and queer studies from California Polytechnic State University, San Luis Obispo. Hannah has written across lifestyle sections including health, wellness, sustainability, personal development, and more. She previously interned for Almost 30, a top-rated health and wellness podcast. In her current role, Hannah reports on the latest beauty trends, holistic skincare approaches, must-have makeup products, and inclusivity in the beauty industry. She currently lives in New York City.